Click HERE to see the CDC recommendation for RSV vaccination for adults
You are about to leave a GSK website
You are about to leave a GSK website. By clicking this link, you will be taken to a website that is independent from GSK. The site you are linking to is not controlled or endorsed by GSK and GSK is not responsible for its content.
OUTCOMES MAY BE SERIOUS FOR ADULTS HOSPITALIZED WITH RSV1-3
Adults who are infected with RSV typically have mild or no symptoms. Symptoms are usually consistent with an upper respiratory tract infection, and mild illness typically lasts 1-2 weeks.4 Some adults, however, may have more severe symptoms consistent with a lower respiratory tract infection, such as pneumonia.5
RSV in hospitalized adults can result in severe outcomes2*
Of 403 patients hospitalized with laboratory-confirmed RSV infection2*:
19.1
of patients had severe clinical outcomes
16.4% admitted to ICU
Median LOS: 7 days
12.4% received mechanical ventilation
Median duration: 3 days
6.7% died in hospital
The most common comorbid conditions were cardiac conditions (47.6%),† respiratory conditions (45.9%),‡ and diabetes (41.4%). Only 4.7% of patients had no comorbid conditions.2
- *
A nested retrospective study using data derived from a prospective surveillance study at 3 academically affiliated hospitals from the same multicampus institution in northern Manhattan identified adults aged ≥18 years who had symptoms of acute respiratory infection and laboratory-confirmed RSV infection from October 2017 through April 2018 and from October 2018 through April 2019. The median age of patients was 69 years. Severe outcomes were defined as ICU admission, mechanical ventilation, and/or in-hospital death.2
- †
Cardiac conditions included CHF, CAD, and/or hypertension.2
- ‡
Respiratory conditions included asthma, COPD, sleep apnea, cystic fibrosis, interstitial lung disease, bronchiectasis, pulmonary fibrosis, and/or pulmonary hypertension.2
Both RSV and influenza have a notable impact on healthcare resource utilization (HRU)3§
In both RSV and influenza, the presence of certain core risk factors (CRFs),‖ including age and comorbidities, can increase HRU.3
HRU as a percentage of patients with and without CRFs
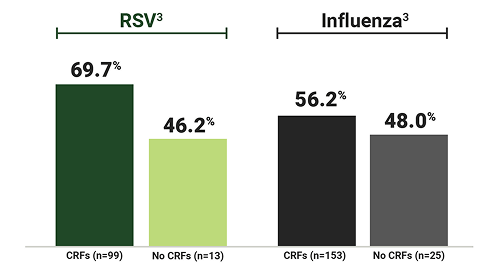
Hospital LOS >3 days¶
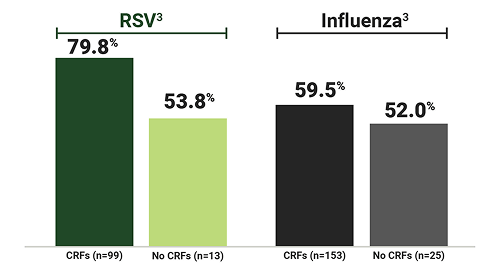
O2 supplementation given
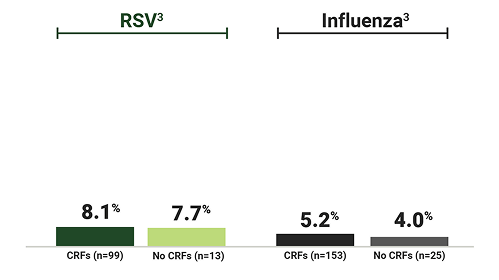
ICU stay
- §
A prospective cohort study assessed adults aged ≥18 years (N=400) who were hospitalized with influenza (n=280) or RSV (n=120) in 5 centers in the United States from 2017 to 2019 for risk factors associated with severe disease. Patients in the RSV cohort were older than those in the influenza cohort (mean: 63.1 years vs 59.7 years), and a higher proportion had CRFs (87.5% vs 81.4%). Healthcare resource utilization assessment included 178 and 112 adults with influenza and RSV, respectively. Clinical information and HRU were collected through clinician-reported questionnaires and through HRU questionnaires during monthly patient phone interviews postdischarge. Clinician-reported questionnaires were not validated against patients’ medical records, and patient-reported HRU was not validated against medical claims data.3
- ‖
CRFs were any one or a combination of the following: age ≥65 years, CAD, COPD, chronic kidney disease, and asthma.3
- ¶
Data from 4 subjects with censored length of hospital stay data were not included in mean (SD) and median (range) results. Censored data included 3 patients with influenza and CRFs (>2, >3, and >6 days) and 1 patient with RSV and CRFs (<3 days).3
Annual healthcare costs can be significantly higher for adults with RSV compared with matched controls6#
Difference in annual healthcare costs for adults with RSV compared with matched controls6
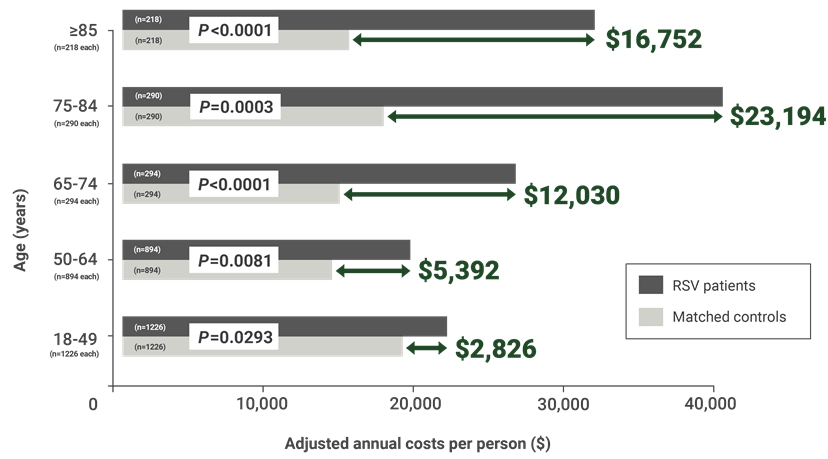
- #
A retrospective case-control study (n=11,432 in each group) used patient data from Truven Health MarketScan Commercial Claims and Encounters, and Medicare Supplemental and Coordination of Benefits databases to identify patients aged ≥1 year with an RSV event between August 31, 2012, and August 1, 2013. Patients with RSV were matched 1:1 with controls based on age, sex, region, health plan, and index date. Patients with RSV had more high-risk comorbid conditions than controls. The number of patients with ≥1 high-risk condition was significantly higher in all age groups with RSV compared with matched controls. Adjusted annual healthcare costs among patients with RSV and matched controls were measured during the follow-up period, with costs adjusted to 2014 US dollars. Associated costs were computed for each resource category and included inpatient, emergency department, ambulatory, outpatient, and prescription medications.6
- Truven Health MarketScan is a registered trademark of Merative US L.P. All other trademarks are owned by or licensed to the GSK group of companies.
CAD=coronary artery disease; CHF=chronic heart failure; COPD=chronic obstructive pulmonary disease; ICU=intensive care unit; LOS=length of stay; O2=oxygen; SD=standard deviation.
References
Branche AR, Saiman L, Walsh EE, et al. Incidence of respiratory syncytial virus infection among hospitalized adults, 2017–2020. Clin Infect Dis. 2022;74(6):1004-1011. doi:10.1093/cid/ciab595
Goldman CR, Sieling WD, Alba LR, et al. Severe clinical outcomes among adults hospitalized with respiratory syncytial virus infections, New York City, 2017–2019. Public Health Rep. 2022;137(5):929-935. doi:10.1177/00333549211041545
Hartnett J, Donga P, Ispas G, et al. Risk factors and medical resource utilization in US adults hospitalized with influenza or respiratory syncytial virus in the Hospitalized Acute Respiratory Tract Infection study. Influenza Other Respir Viruses. 2022;16(5):906-915. doi:10.1111/irv.12994
Respiratory syncytial virus infection (RSV). Clinical overview of RSV. Centers for Disease Control and Prevention. Accessed July 8, 2025. https://www.cdc.gov/rsv/hcp/clinical-overview/index.html
Respiratory syncytial virus infection (RSV). RSV in adults. Centers for Disease Control and Prevention. Accessed July 14, 2025. https://www.cdc.gov/rsv/adults
Amand C, Tong S, Kieffer A, Kyaw MH. Healthcare resource use and economic burden attributable to respiratory syncytial virus in the United States: a claims database analysis. BMC Health Serv Res. 2018;18(1):294. doi:10.1186/s12913-018-3066-1
